
Cancer is one among many non-communicable diseases (NCDs) that enjoy an unprecedented global profile. Yet, of the 4 billion people living in cities and urban areas, only a few have access to high-quality cancer treatment, particularly in low- and middle-income countries (LMICs). One contributing factor is the significant gender gap in oncology practice, particularly in LMICs. Despite the growing number of women practising medicine globally, oncology remains male-dominated, limiting the presence of women in leadership, research, and specialized cancer care. This lack of gender diversity can affect healthcare policies, research priorities, and patient outcomes, further exacerbating disparities in access to quality treatment.
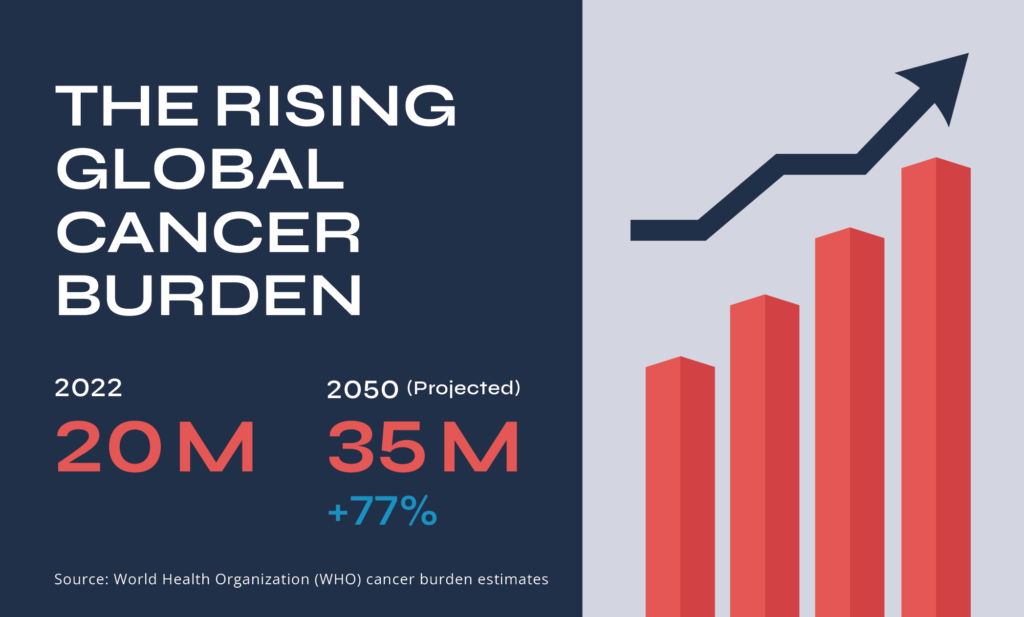
Nowhere is this challenge more evident than in Africa, where the rising cancer burden is further deepened by an acute shortage of oncology professionals. If current trends persist, an estimated 1,000,000 cancer-related deaths will occur annually in sub-Saharan Africa. Increasing the oncology workforce particularly by addressing gender disparities and supporting more women to enter and advance in oncology is critical to mitigating this crisis, as Africa currently experiences the highest health workforce deficits in the world, including in oncology with women constituting 67.2% of the health workforce yet hold only 25% of senior roles.
With this in mind, City Cancer Challenge (C/Can) in collaboration with ASCO has developed the Leadership Programme for Women in Oncology (LPWO), now in its second edition. This initiative equips mid-career women oncologists from C/Can cities with the leadership skills needed to drive change in cancer care, envisioning a future where access to quality treatment is not determined by gender, geography, socioeconomic status, or identity.
In January, Abuja was selected to host the global launch of the programme in collaboration with the Federal Ministry of Health, featuring nine mid-career women oncologists from nine countries. For Nigeria, where the burden of cancer continues to rise, the urgency of such leadership has never been greater. Dr Adedolapo Fasawe, Mandate Secretary for Health Services and Environment Secretariat at the Federal Capital Territory, highlights the importance of investing in capacity building for oncology professionals.
By equipping talented professionals with the skills to drive innovation and collaboration in oncology, we are investing in a future where all perspectives contribute to effective and equitable cancer care solutions

Closing the gender gap in oncology
In oncology, this gap is particularly concerning given the significant impact of cancer on women’s health—breast and cervical cancer remain among the most prevalent globally. Despite this, women oncologists, especially in LMICs, are often excluded from decision-making processes that shape the system. Their perspectives, experiences, and leadership are essential for driving meaningful change.
A report by The Lancet Commission on Women, Power, and Cancer highlights how social inequalities put women at higher risk of cancer and limit their access to diagnosis and care. It stresses that factors like gender, age, and income affect cancer outcomes and calls for policies that address these disparities. Women also take on most unpaid caregiving and face barriers in advancing their careers in healthcare and research.
Breaking barriers in oncology
The gender gap in oncology is reinforced by structural and societal barriers that limit women’s entry and advancement in the field. Limited mentorship and leadership opportunities, gender biases in medical education and hiring, work-life balance challenges, and restricted access to research funding all contribute to this imbalance. As a result, many talented women are discouraged from pursuing careers in oncology, and those who do often face obstacles to reaching senior positions.

Key goals for the second cohort
- Strengthening female leadership in oncology
Top on the list of gender equity in cancer care is the representation of women in leadership roles. The LPWO provides structured leadership training, equipping female oncologists with decision-making, strategic planning, and advocacy skills. With more women stepping into leadership positions, policies and programs will become more inclusive and responsive to diverse patient needs.
- Enhancing access to cancer care
Addressing the complexities of global cancer control will require diverse teams to create solutions tailored to different contexts. Having more women in leadership is crucial for gender equity in healthcare. Breaking barriers like the glass ceiling and the leaky pipeline will help retain talent, improve workplace culture, and ensure cancer care systems are gender-responsive. - Expanding mentorship and capacity building
The lack of mentorship for young female doctors pursuing oncology careers is a critical gap. The LPWO creates a network of trained women leaders who can mentor, train, and inspire the next generation of female oncologists. This not only helps bridge the gender gap but also expands the oncology workforce, addressing the shortage of specialists in LMICs.
Advancing Gender-Inclusive Cancer Control in Nigeria
To enhance the effectiveness of Nigeria’s cancer control efforts, gender balance must be prioritised in both policy formulation and implementation. While the National Strategic Cancer Control Plan 2023-2027; the National Cancer Research Agenda 2024-2028, and the National Strategic Plan for Prevention of Cancer of Uterine Cervix 2023-2027 outline critical steps for cancer prevention, treatment, and research, they do not explicitly address gender disparities in cancer care leadership and workforce representation.
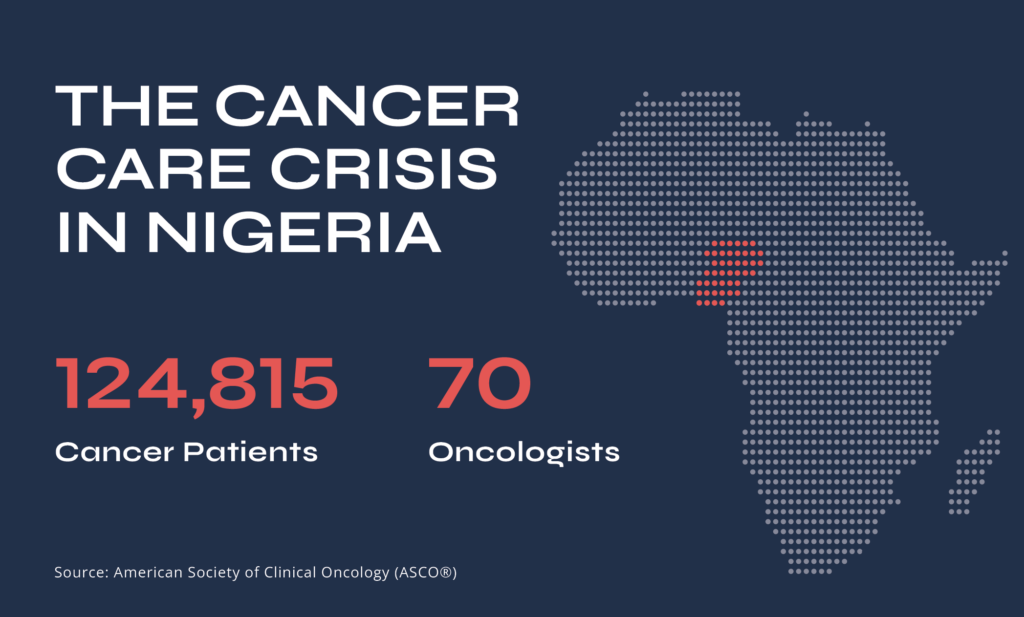
Moving forward, Nigeria can take a more gender-inclusive approach by setting targets for female representation in leadership roles and strengthening mentorship and training programmes through scholarships and research grants for women in oncology.
Advocacy efforts should also emphasise the importance of gender inclusion in cancer care and leadership, engaging policymakers, and stakeholders to drive sustainable change.
By integrating these measures into Nigeria’s cancer control framework, the country can build a more inclusive, skilled, and effective oncology workforce, one that reflects the diverse perspectives needed to improve cancer outcomes for all.
We thank Roche for their continued support of the LPWO programme and its in-kind collaboration in providing mentorship to its cohorts.






